3D-bioprinting, a state-of-the-art technology similar to 3D-printing, uses digital files as blueprints to create living tissues layer-by-layer. Bio-printers use cells and biomaterials to create organ-like structures which let living cells multiply.
This rapid-prototyping can create living tissue, blood vessels, bone, skin, and whole organs such as the heart, making 3D-bioprinting a game changer in the future of medicine. Bioprinting has the potential of eradicating organ transplantation waiting lists by eliminating organ shortage.
In addition, 3D-bioprinting can potentially end lab animal testing; miniature organs and patient-specific bioprinted tissue –such as heart tissue– could be used instead, eliminating rejections and animal cruelty.
In the last five years, scientists have been able to bioprint a heart, lungs, skin, kidneys, and corneas. Looking further into the future, we could see fully functioning organs within a decade, with major implications in regenerative and cosmetic medicine.
Leading pioneer companies in the tissue engineering field, such as Swedish CELLINK, the first bio-ink company, and California-based Organovo , are currently offering their technologies onto the market, addressing the need for 3D-printed human tissue for medical research and pharmaceutical drug discovery.
Christopher Barnatt, futurist, speaker, and author of several books on future technologies and future trends including 3D-Printing, 25 Things You Need to Know about the Future, and creator of ExplainingTheFuture.com, anticipates that bioprinting will trigger a medical revolution in the course of this decade and beyond.
“By the late 2020s, I expect bioprinting to be used to create small soft tissues, like nerve and arterial grafts and liver matches, for human transplantation. By the early 2030s, I expect we will see the transplantation into a human of the first bioprinted kidney, and then later that decade maybe a pancreas,” Barnatt tells Navigate the Future.
Barnatt believes that thanks to bioprinting, replacement organs will be output to each individual patient specification and every item printed will be created from a culture of a patient’s own cells, the risk of transplant organ rejection should be very low.
“One day, we are likely to be able to bioprint a heart, but it is a more complex challenge than simpler organs like a kidney. The issues faced are two-fold. Firstly, there is the need to keep thick tissues alive during the bioprinting process, and this requires some kind of temporary vascular network to be in place,” Barnatt says.
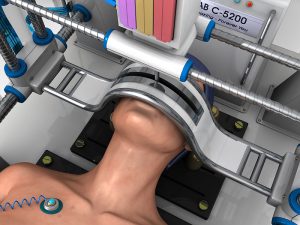
“Secondly, even when we can bioprint thick tissues like heart muscles, they are unlikely to be strong enough for immediate functional use. A natural heart has grown over time, beating and hence being exercised for years. So, it is likely that a bioprinted heart will need exercising to strengthen its muscle tissues before transplantation. So, we may need robotic exercise machines for some bioprinted organs.”
On the subject of modeling, Barnatt says that one of the fascinating aspects of bioprinting is that it is a naturally biological as well as an artificial additive layer manufacturing process.
“What bioprinters do is to put roughly the right cells in roughly the right places. But then nature takes over to re-arrange the cells and to join them into cohesive living tissue. This means that, for example, there is no need to model all of the capillaries in the kidney in order to bioprint it, as this level of detail occurs naturally once bulk cell placement has been achieved via a bioprinting process,” he says.
The future of medicine: From printing a new face to in-situ bioprinting
According to Barnatt, keyhole bioprinters may one day repair organs. A combination of 3D modeling and a 3D face bioprinter may make the dream of eternal youth a reality. For Christopher Barnatt, a face printer, a future kind of in-situ bioprinter, will be able to evaporate existing cells from the face and replace them with new cells to patient specification.
Face bioprinting may raise ethical and security concerns, though. Only time will tell to what extent humanity will be mature enough to take advantage of using advanced technologies in a responsible and ethical manner. Most immediate applications in reconstructive medicine include chronic wounds such as diabetic, venous and pressure ulcers, and burn wounds which represent a burden to patients and surgeons alike. These wounds affect over 7 million patients in the United States alone, with an annual treatment expenditure of over $25 billion.
Chronic, large, or non-healing wounds are especially costly since they often require multiple treatments. A single diabetic foot ulcer can cost approximately $50,000 to treat. Full thickness skin injuries make up for a major source of mortality and morbidity for civilians.
It is estimated that 500,000 civilian burns are treated in the United States each year. For military personnel, burn injuries account for 10–30 percent of combat casualties in conventional warfare.
A bioprinter equipped with a built-in laser scanner can scan a wound and determine its depth and area. Following this, the scan is converted into 3D digital images which enable the device to calculate how many layers of skin cells would need to be printed on the wound in order to restore it to its original configuration.
In the future, bioprinting technology will potentially contribute to other new biotechnologies for advanced organ transplants and gene therapy.